Introduction
The convenience of seeing online doctors from your couch feels like a modern miracle. No waiting rooms, no commutes, and a prescription in minutes.
But beneath the glowing interface of your favorite telehealth app lies a silent, growing danger that medical boards are only just beginning to whisper about.

The Invisible Wall: What Online Doctors Simply Cannot See
We’ve become addicted to the “Uber-fication” of healthcare. We want our diagnosis as fast as our DoorDash delivery.
However, online doctors are operating with one hand tied behind their backs. There is a fundamental human element—a physical reality—that technology has yet to replicate.
The “One Thing” they can’t do? The Comprehensive Physical Palpation.
It sounds technical, but it’s the difference between life and death. An online doctor cannot feel the hidden lump behind your ear, the subtle rigidity of an abdomen, or the coldness of a limb that signals poor circulation.
Why the “Digital Gap” is Widening
When you consult with online doctors, you are providing the data. You are the eyes, the ears, and the hands of the physician.
If you miss a symptom, they miss the diagnosis. This creates an online doctors risk that most patients don’t realize they are signing up for.
The Expert Warning: Why “Convenience” is a Double-Edged Sword
Leading health organizations are sounding the alarm. While telehealth is a “godsend” for rural areas, the over-reliance on it for complex issues is dangerous.
According to a recent report by the American Medical Association, the lack of a physical exam is one of the primary drivers of diagnostic error in virtual settings.
The Risks You Aren’t Told About:
-
Missing “Silent” Symptoms: Many life-threatening conditions (like early-stage heart murmurs) show no symptoms you can feel, but a doctor can hear.
-
Over-Prescription: To compensate for a lack of physical data, some online doctors may over-prescribe antibiotics or steroids.
-
Fragmented Care: Your virtual doctor often doesn’t have access to your full local medical records.
“The screen acts as a filter. It filters out the smell of an infection, the subtle tremor of a hand, and the nuance of a patient’s gait.” — Dr. Elena Rossi, Medical Safety Advocate.
The Evolution of Telehealth: How We Got Here
To understand the current online doctors risk, we have to look at the history of the industry. Telehealth didn’t start with apps; it started with radio.
In the early 20th century, ships at sea used radio to consult with doctors on land. It was a matter of survival. Fast forward to the 2020 global shift, and suddenly, everyone from pediatricians to psychiatrists moved to Zoom.
The Gold Rush of Virtual Care
The market for online doctors exploded virtually overnight. This led to:
-
Venture Capital Influx: Huge amounts of money poured into platforms that prioritize “user acquisition” over clinical depth.
-
The Gig Economy for MDs: Many doctors working these platforms are doing so as a “side hustle,” seeing 20+ patients an hour.
-
Regulatory Lag: Laws haven’t caught up to the speed of the software.
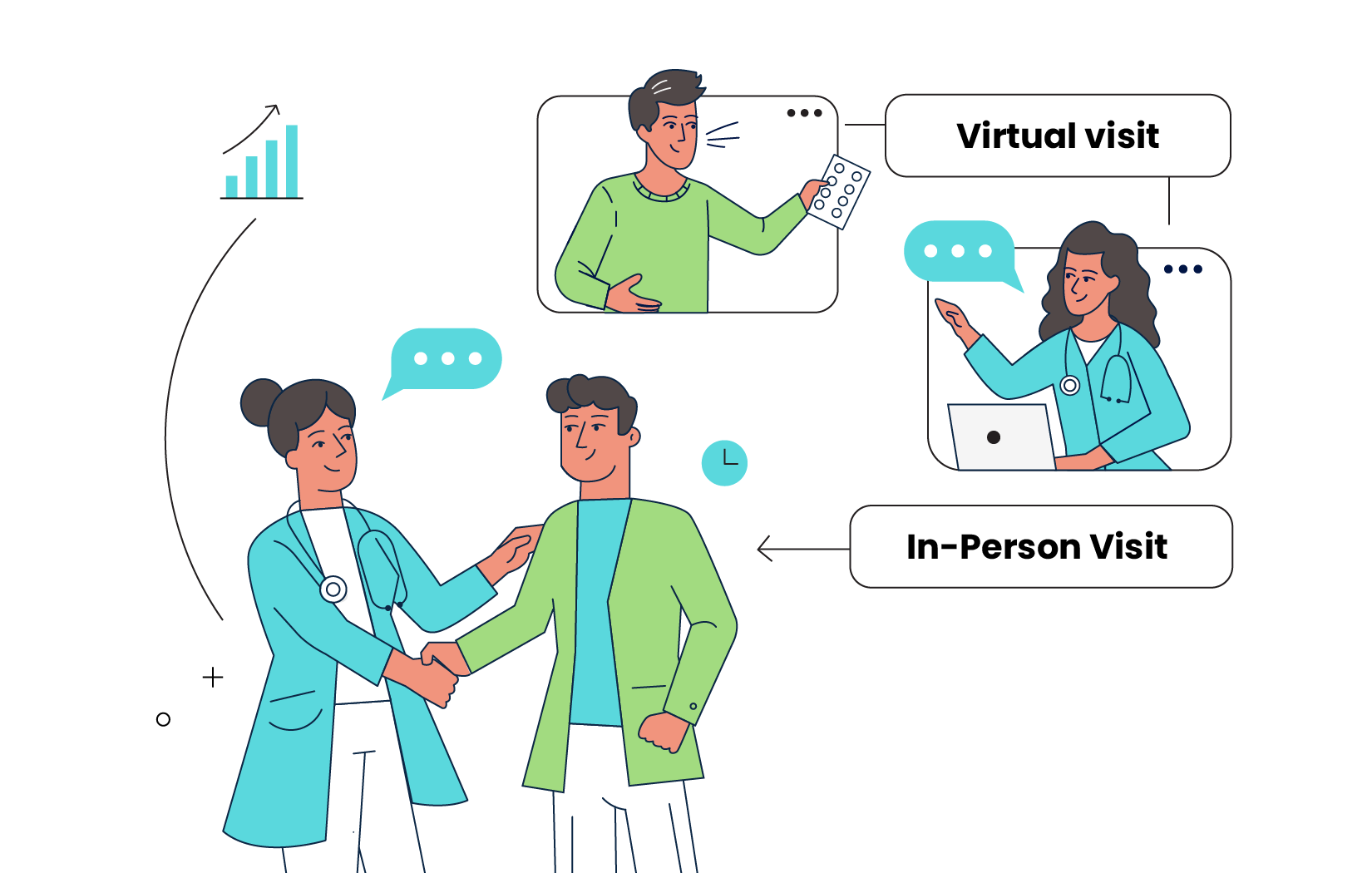
Comparing the Experience: Virtual vs. In-Person Care
To understand the online doctors risk, we have to look at what is gained and what is sacrificed.
| Feature | Online Doctors | In-Person Doctors |
| Speed | Instant / Same Day | Days or Weeks |
| Physical Exam | Visual Only | Comprehensive / Tactile |
| Diagnostic Accuracy | High for Simple Issues | High for All Issues |
| Cost | Usually Lower | Usually Higher |
| Travel Required | None | Yes |
| Risk Factor | Potential for Missed Physical Cues | Low |
The Dangerous Anatomy of a Virtual Appointment
When you log on to see online doctors, a clock starts. Most platforms incentivize short call times. This pressure creates a dangerous environment for diagnostic errors.
The Missing “Five Senses” in Medicine
A traditional doctor uses almost all their senses. Online doctors are limited to only two: sight and hearing (and even those are compressed by low-resolution internet connections).
-
Smell: Did you know certain infections or ketoacidosis have distinct smells? A screen blocks this entirely.
-
Touch (Palpation): This is the “One Thing.” Feeling for enlarged organs or the texture of a skin lesion.
-
Hearing (Auscultation): Unless you have a digital stethoscope at home, the doctor cannot hear your heart or lungs.
Specific Case Studies: When the System Fails
To truly grasp the online doctors risk, we must look at real-world scenarios where the “digital wall” caused harm.
Case #1: The “Simple” Skin Rash
A patient consulted online doctors for a red patch on their leg. Through a webcam, it looked like cellulitis. The doctor prescribed antibiotics. In reality, it was a deep vein thrombosis (a blood clot). Because the doctor couldn’t “feel” the heat or the specific type of swelling, the patient nearly suffered a pulmonary embolism.
Case #2: The Abdominal “Cramp”
A young man reported stomach pain via a popular app. The doctor suggested it was food poisoning. Hours later, his appendix burst. An in-person doctor would have performed a “rebound tenderness” test in 5 seconds and sent him to surgery.
Case #3: The Mental Health Oversight
While online doctors are great for therapy, they can miss the physical “tells” of medication side effects, such as the subtle muscle twitching (tardive dyskinesia) that signals a dangerous reaction to antipsychotics.
The Psychological Trap of the “White Coat Screen”
There is a documented psychological effect where patients are less honest with online doctors.
Because we are in our own homes, we feel a false sense of security. We might downplay symptoms because we don’t want to be told to go to the hospital. Conversely, doctors may feel less “connected” to the patient, leading to a decrease in clinical empathy.
The Technical Failures: Resolution and Lag
Even the best online doctors are at the mercy of your Wi-Fi.
-
Color Distortion: A sore throat might look “angry and red” under a cheap LED bulb but normal in person.
-
Audio Compression: A wheeze in the lungs can be filtered out by noise-canceling software intended to “clean up” the call.
-
Lag: Small neurological “lag” in a patient’s facial expressions (a sign of a stroke or palsy) can be mistaken for internet jitter.
Red Flag Symptoms: When Online Doctors Are NOT Enough
If you are using online doctors, you must know when to close the laptop and head to an ER or a local clinic.
1. Shortness of Breath
This is non-negotiable. This requires a lung auscultation that a phone microphone cannot replicate. It could be pneumonia, heart failure, or a clot.
2. Unexplained Weight Loss
This often requires physical palpation of the thyroid and abdomen. Virtual doctors cannot feel for “hard” masses in the gut.
3. Sudden, Severe Headaches
Often dismissed as “migraines” over video calls, these require physical neurological testing to rule out an aneurysm.
4. Severe Abdominal Pain
An online doctor cannot perform a “rebound tenderness” test to check for appendicitis. If it hurts when they let go of the pressure, you need surgery.
How to Minimize the Online Doctors Risk (A Step-by-Step Guide)
You don’t have to quit telehealth. It is an incredible tool when used correctly. Here is how to protect yourself:
Step 1: Be Your Own Medical Assistant
Before your call with online doctors, take your own vitals if you have the equipment.
-
Check your temperature.
-
Measure your heart rate (using a smartwatch or the pulse in your neck).
-
Use a home blood pressure cuff.
-
Record your weight.
Step 2: Lighting and Environment
If you are showing a rash or a wound to online doctors, use natural sunlight near a window. LED bulbs can distort colors, leading to a misdiagnosis. Turn off all background noise so the doctor can hear your voice clearly.
Step 3: The “Paper Trail”
Always ask for a copy of the “Clinical Note” from the session. Ensure your primary care physician (PCP) receives a copy. The Mayo Clinic’s guidelines on patient advocacy emphasize that fragmented records are a leading cause of medical error.
Step 4: Demand a Referral
If an online doctor suggests a “wait and see” approach for a physical symptom, push for a local referral. If you feel something is wrong, trust your gut—not the screen.
The Rise of “Hybrid Health”
The future isn’t just “online” or “in-person.” It is “Hybrid.”
Experts are now pushing for a model where online doctors are the “triage” center. You call them first, and they determine if your issue is “Digital-Safe” or “Physical-Required.”
Digital-Safe Conditions:
-
Prescription refills (non-controlled)
-
Mild allergies
-
Cold/Flu (without breathing issues)
-
General mental health check-ins
-
Follow-up results for blood work
Physical-Required Conditions:
-
New, undiagnosed pain
-
Lumps or growths
-
Heart palpitations
-
Pregnancy-related concerns
The Legal Landscape: Who Is Responsible?
When things go wrong with online doctors, finding accountability is difficult.
Many telehealth companies are structured as “technology platforms,” not “medical groups.” This creates a legal gray area if a misdiagnosis occurs.
-
Jurisdiction Issues: If you are in Florida and the doctor is in California, which state’s laws apply?
-
Standard of Care: Courts are still deciding if the “Standard of Care” for an online doctor is lower than that of an in-person doctor due to the inherent limitations of the tech.
Technology to the Rescue? The Next 5 Years
Can we solve the online doctors risk with more tech? We are trying.
1. Peripheral Telehealth Kits
Companies are developing home kits that include:
-
Digital stethoscopes that stream your heartbeat to the doctor.
-
High-definition otoscopes for ear exams.
-
Dermatoscope attachments for high-res skin photos.
2. AI Symptom Checkers
AI is being integrated into the “waiting room” of online doctors. The AI asks 50 questions before the doctor even joins, ensuring no stone is left unturned.
3. Wearable Data Integration
In the near future, your online doctors will see a dashboard of your last 30 days of heart rate, sleep, and oxygen levels via your Apple Watch or Oura Ring.

FAQ: Your Most Urgent Questions Answered
Can online doctors prescribe any medication?
No. Most online doctors are legally restricted from prescribing “controlled substances” (like Xanax, Adderall, or OxyContin). If a site claims they can do this without a rigorous exam, it is likely an illegal “pill mill.”
Is my data safe with online doctors?
Generally, yes, provided the platform is HIPAA-compliant. However, you should always check the privacy policy. Avoid using free video apps like Skype or FaceTime for medical consults; only use dedicated, encrypted health platforms.
What is the biggest online doctors risk?
The biggest risk is “Misattribution.” This happens when a doctor attributes a serious physical symptom (like a heart issue) to a minor condition (like anxiety) because they cannot physically examine the patient.
Do online doctors take insurance?
Most major platforms now take insurance, but you should always verify “In-Network” status before the call to avoid a surprise $150 bill.
Can online doctors give me a sick note for work?
Yes, most can provide a legitimate medical excuse note for short-term illnesses like the flu or a cold.
The Expert Verdict: Use with Caution, Not Fear
We are not suggesting you stop using online doctors. They have revolutionized access for those in rural areas and for those with mobility issues.
However, we must move past the “honeymoon phase” of telehealth. We must acknowledge that a camera lens is not a substitute for a doctor’s touch.
The Rule of Thumb: If you can see it, hear it, or talk about it—telehealth is great. If you have to feel it—go to the clinic.
Conclusion: Protecting Your Health in a Digital World
The online doctors risk is a manageable one, provided you are an informed patient. Use virtual care for convenience, but never sacrifice your safety for a shorter wait time.
Your health is the most valuable thing you own. Don’t let a “connection error” be the reason you miss a life-changing diagnosis.
What should you do next?
If you have a persistent physical symptom that you’ve only discussed with online doctors, schedule an in-person “wellness check” this week. It might just save your life.
Was this helpful?
Share This Article With a Friend Who Uses Telehealth
Read More: