Introduction
You use telehealth apps for speed and convenience — but a hidden loophole in how many platforms operate could leave you exposed. This tiny flaw can cost you money, your privacy… even your health.
Quick note: this post draws on guidance and investigations from trusted sources (CMS, HHS, peer-reviewed studies and major news outlets) to explain the loophole, show real-world consequences, and give step-by-step protections you can act on now. CMS+1
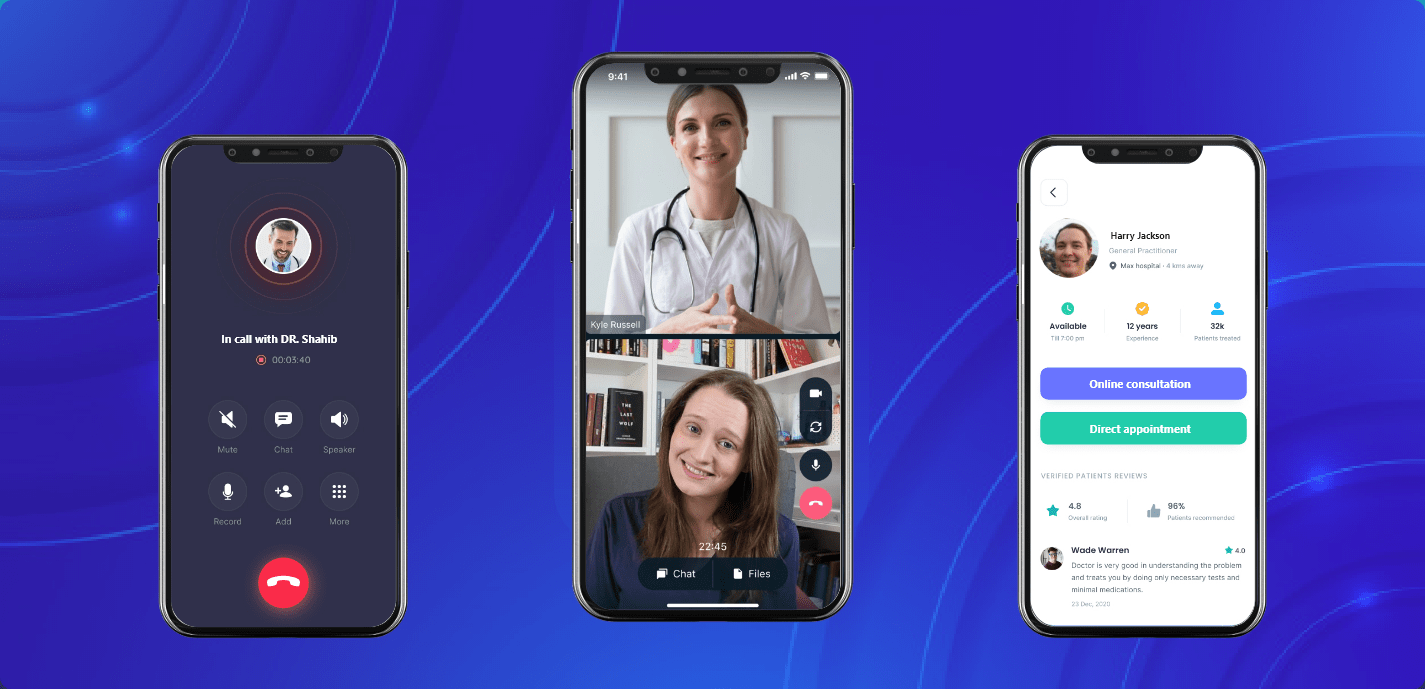
Why this matters: the telehealth promise vs. the messy reality
Telehealth apps exploded during the pandemic and have stayed because they work: faster access, less travel, and (often) lower immediate cost. But convenience created incentives and technical shortcuts — and some of those are where the loophole lives.
Short version: many telehealth platforms, third-party vendors, and fragmented billing flows create gaps. These gaps can let providers or platforms bill unexpectedly, share sensitive data, or prescribe controlled drugs under flexible rules — sometimes in ways regulators and patients didn’t intend. CMS+1
What is the Telehealth App Loophole?
The “Telehealth App Loophole” is not a single law or bug. It’s a cluster of operational and regulatory gaps that allow:
-
Surprise or out-of-network billing through complex referral chains and vendor markup.
-
Data sharing outside HIPAA protections when apps use third-party trackers or aren’t fully covered by HIPAA.
-
Prescribing and supply-chain abuses, where telemedicine visits become a pipeline for overprescribing or unnecessary durable medical equipment (DME). CMS+2AP News+2
Why “loophole” and not “fraud” only? Because some of these gaps are legal, or a result of inconsistent laws — not outright criminal schemes (though fraud can and does occur). Regulators have taken notice, and enforcement is increasing. CMS+1
Three common faces of the loophole
-
Balance-billing and surprise charges — You think you paid the telehealth copay. Later a specialist or platform bills you out-of-network. The federal No Surprises Act sought to fix surprise billing — but telehealth billing chains can still create confusion. CMS+1
-
Data leakage through ad-tech and SDKs — Apps that collect health info may embed analytics/advertising SDKs that share identifiable or sensitive data with ad networks. Not all health apps are fully covered by HIPAA (for example, many consumer-facing apps). Enforcement actions (e.g., GoodRx, Premom) show regulators are watching. AP News+1
-
Regulatory flexibilities for controlled substances — Emergency/temporary rules and DEA flexibilities have expanded tele-prescribing for controlled drugs (e.g., some GLP-1 weight-loss drugs, opioids historically). That can be medically appropriate but also opens the door to overprescribing and platform-driven volume. Recent DEA/HHS guidance extended some telehealth prescribing flexibilities, and Congress/regulators are actively updating frameworks. Federal Register+1
Real risks: not just dollars (why “more than money”)
This loophole can cost you in three major non-monetary ways:
Privacy & future harm
-
Health details leaked to ad networks or data brokers can be permanent. That data might be used to target you, deny services, or — in some jurisdictions — be used in criminal or civil investigations (examples: reproductive health data concerns). FTC and other agencies have fined and sanctioned companies for improper data sharing. AP News+1
Clinical safety
-
Fragmented care and telehealth-for-volume models can result in inappropriate prescriptions, missed comorbidities, or lack of follow-up. The CMS white paper highlights fraud/waste patterns tied to telehealth growth — including unnecessary DME or prescriptions. CMS
Legal / insurance exposure
-
Out-of-network bills, denied claims, and state-level variations in telehealth law can leave patients facing surprises despite thinking they followed insurer rules. The No Surprises Act reduces certain risks, but nuances remain. CMS
Hard evidence: what the reports and regulators say
-
The Centers for Medicare & Medicaid Services studied telehealth-related fraud, waste, and abuse and warns that analytics and cross-platform referral chains make detection tricky. CMS
-
Peer-reviewed reviews find telehealth privacy and security risks are real, particularly where apps or platforms use third-party services and lack robust encryption/controls. PMC
-
HHS guidance explains conditions under which controlled substances can be prescribed via telehealth — and how temporary flexibilities have been extended, but remain subject to regulation. telehealth.hhs.gov+1
These are load-bearing findings: regulators see problems, research documents risks, and federal rules have been adjusted — which means the loophole is real and evolving. CMS+1
Table: Telehealth App Loophole — Scenarios, Consequences, and How to Spot Them
| Scenario (what happens) | Main consequence(s) | How to spot it (red flags) | Quick fix / what to ask |
|---|---|---|---|
| App visit billed, later an out-of-network bill appears | Unexpected charges, denied claims | Different provider names on bills; provider not listed in your insurer’s portal | Ask insurer if telehealth provider is in-network before visit |
| App uses embedded ad SDKs or trackers | Sensitive health data shared with advertisers | App privacy policy vague; presence of many trackers; third-party cookies | Check privacy policy, request data deletion, prefer HIPAA-covered providers |
| Tele-prescribing of controlled meds with minimal follow-up | Overprescribing, medication mismatch | Rapid prescription approval, limited medical record history | Request medication rationale, ask for follow-up plan |
| Platform sends DME (braces, supplies) after tele-visit | Unneeded equipment; billing fraud | Unsolicited supply shipments after visit | Refuse unsolicited supplies; confirm orders in writing |
| Multi-vendor chain: platform, telehealth doctor, DME provider | Hard to contest bills, fragmented accountability | Multiple company names on records; confusing T&Cs | Save all communications; escalate to insurer or state consumer agency |
| *(Sources: CMS, HHS, peer-reviewed privacy studies and recent enforcement actions). * CMS+2telehealth.hhs.gov+2 |
How tech and business models created the loophole
Telehealth companies often stitch together many services:
-
Clinician networks (often contractors)
-
Platform infrastructure (video, scheduling) supplied by vendors
-
Pharmacy partnerships or tele-pharmacies
-
Analytics and monetization (ads, data-sharing)
This modular architecture speeds growth but also spreads liability and obscures responsibility. When something goes wrong — a surprise bill, data leak, or questionable prescription — each party can point at the other. Regulators and payers pay attention to the whole chain, but patients often do not. CMS+1
Step-by-step: How to protect yourself from the Telehealth App Loophole
Use this checklist before, during, and after any telehealth visit.
Before booking
-
Confirm the provider is in-network with your insurer (ask for the clinician’s NPI or business name).
-
Read the app’s privacy policy — search for words like “sharing,” “third parties,” “tracking SDK,” and “HIPAA.” If it’s vague, ask. AP News
-
Prefer platforms that explicitly say they are HIPAA-compliant and list business associate agreements.
During the visit
-
Ask the clinician to state their name, license, and state of licensure on the record.
-
Ask about follow-up plans, how prescriptions will be handled, and whether any supplies will be ordered on your behalf.
-
Don’t provide extra personal data (precise geolocation, photos of non-essential documents) unless necessary.
After the visit
-
Save any receipts, transcripts, or prescriptions.
-
Watch your insurer’s explanation of benefits (EOB) for unexpected charges — and compare names on the EOB to the app and clinician.
-
If you get unsolicited DME or strange charges, refuse the shipment and contact your insurer + the platform. Report suspicious activity to your state consumer protection office or the FTC. CMS+1
What to ask tech vendors and apps (script you can copy)
-
“Are you a covered entity under HIPAA or do you have a Business Associate Agreement (BAA) with my clinician?”
-
“Do you share user data with third-party ad platforms or analytics providers?”
-
“How do you handle prescriptions and DME orders? Who signs off and what oversight exists?”
-
“Which state(s) are your clinicians licensed in?”
If the app stalls or gives a corporate-speak answer, treat that as a red flag.
Policy & regulatory landscape: what’s changing (and what that means)
Regulators are moving fast because the telehealth industry is changing fast.
-
Surprise billing: The No Surprises Act addressed many emergency and facility-based surprise bills, but telehealth billing practices still need vigilance. Patients should verify network status before a visit. CMS
-
Data enforcement: The FTC has stepped in where HIPAA does not apply, fining or enforcing against apps that mislead users about data practices (GoodRx and fertility apps are examples). Expect more enforcement and possibly new federal rules aimed at consumer health apps. AP News+1
-
Prescribing rules: DEA/HHS temporary flexibilities for controlled substances have been extended in recent years; regulators are debating how and whether to make some flexibilities permanent while balancing access and safety. That affects tele-prescribing of medications like GLP-1 drugs and controlled psychotropics. Federal Register+1
These policy shifts mean platforms will need better compliance, and users should expect clearer disclosures and stronger privacy controls over the next few years.
Case studies: real-world examples (what actually happened)
Case 1 — Data sharing and targeted ads (consumer app)
A popular prescription discount/telehealth ecosystem faced enforcement over sharing user health data with ad platforms. The resulting settlement and publicity forced changes in privacy controls — but showed how even well-known players can mishandle sensitive info. AP News
Case 2 — Telehealth DME spike and fraud
Past telehealth expansions led to increases in fraudulent DME claims and unnecessary supplies. CMS and oversight bodies documented schemes where telehealth visits were used to authorize unnecessary orders, demonstrating the risk when oversight is weak. CMS
Case 3 — Rapid tele-prescribing growth (GLP-1s)
The telehealth boom in weight-loss drugs (GLP-1s) surged demand and attracted many platforms. Journalistic reporting highlighted privacy and cross-state prescribing questions, prompting calls for clearer guardrails. Reuters
Each case shows that convenience without guardrails produces harms — financial, clinical, and privacy-related.
Comparison table: Safe Telehealth vs. Risky Telehealth
| Feature | Safe Telehealth (what to look for) | Risky Telehealth (red flags) |
|---|---|---|
| Network status | Clinician clearly in-network; insurer confirms | Unknown provider; later EOB shows out-of-network |
| Privacy | App lists HIPAA compliance, BAA, minimal third-party SDKs | Vague privacy policy; many trackers or ad partnerships |
| Prescribing | Clear follow-up, documented medical history, local licensure | Rapid prescriptions without clear record or local licensure |
| Billing transparency | Upfront estimate; single recognizable billing entity | Multiple vendor names; surprise bills later |
| Vendor accountability | Public provider credentials; customer support and escalation | Hard-to-reach support; T&C pass liability to multiple vendors |
(Derived from CMS reports, HHS guidance, and privacy enforcement cases). CMS+2telehealth.hhs.gov+2
How industry and clinicians can fix the loophole
-
Stronger vendor transparency: platforms must disclose trackers, data flows, and business relationships plainly. (Regulators already pushing here.) AP News
-
Clear billing flows: unified billing identifiers so patients know who will bill them — and how to contest. CMS guidance and payer audits can accelerate this. CMS+1
-
Clinical guardrails: telehealth should include minimum documentation, clear follow-up, and prescriber accountability, especially for controlled substances. HHS guidance shows this is already a regulatory focus. telehealth.hhs.gov
-
Better patient education: simple prompts in apps that explain privacy, billing, and prescribing practices in plain language.
These steps reduce the loophole’s impact and restore patient trust.
FAQs about the Telehealth App Loophole
Q1 — Is the Telehealth App Loophole illegal?
Not always. Many loophole aspects are legal gaps or inconsistent rules rather than explicit illegality. But when a platform or provider commits fraud or violates privacy laws, enforcement follows. Learn more from CMS and the FTC on reporting and protections. CMS+1
Q2 —Can my insurer protect me against surprise telehealth bills?
Yes and no. Federal rules (No Surprises Act) and some state laws protect consumers in many cases — but you should always confirm the clinician is in-network before a visit. CMS
Q3 —Do all telehealth apps have poor privacy practices?
No. Many reputable health systems and covered entities follow HIPAA and strong privacy practices. The risk is higher with direct-to-consumer apps that monetize via advertising or data sharing. Check privacy policies and prefer BAAs. AP News
Q4 —What should I do if I get an unexpected bill or receive suspicious supplies?
Save records, contact the platform, contact your insurer, and if unresolved report to state consumer protection offices and the FTC. CMS and state resources offer dispute pathways. CMS+1
Q5 —Are prescriptions through telehealth safe?
Often yes — many conditions are safely managed via telehealth. But be alert for rapid prescribing without proper assessment or follow-up. For controlled substances, ask about the clinician’s evaluation process and licensure. telehealth.hhs.gov
Action plan: 7 things to do after reading this
-
Audit apps on your phone: uninstall apps you don’t use; review privacy settings.
-
Check the clinician’s NPI: ask the telehealth provider for their NPI (National Provider Identifier) and confirm licensure.
-
Verify in-network status: call your insurer before high-cost visits.
-
Use established systems: prefer hospital/health-system portals over fly-by-night apps.
-
Limit personal data sharing: avoid unnecessary uploads of sensitive docs or location tags.
-
Monitor EOBs closely: compare EOB entries with your visit receipt.
-
Report when needed: unexpected charges or privacy breaches should be reported to insurers, CMS (if Medicare/Medicaid), and consumer protection agencies. CMS+1
Tools & resources (trusted places to learn more)
-
CMS — No Surprises Act & telehealth guidance — explains consumer protections around surprise bills. CMS
-
HHS Telehealth Policy — practical guidance on tele-prescribing and controlled substances. telehealth.hhs.gov
-
NIH / NCBI research on telehealth privacy — peer-reviewed analyses of privacy and security risk factors. PMC
-
Recent journalism on GLP-1 and telehealth privacy — coverage of industry trends and regulator concerns. Reuters
(Clicking these resources will give you the primary-source context regulators and patient advocates use.)
The future: will the loophole close?
Short answer: likely yes — but slowly. Expect:
-
More FTC / HHS enforcement against improper data practices. AP News
-
Clearer tele-prescribing guardrails balancing access and safety. Federal Register
-
Platform-level changes: better transparency, fewer trackers, and stronger BAAs for clinical integrations.
Until then, patient vigilance and smarter platform choice remain the best defense.
Conclusion: convenience without vigilance is risky
Telehealth apps have changed healthcare for the better — but the Telehealth App Loophole shows how speed + layered business models can introduce hidden harms. Money is the easiest damage to spot; privacy loss, clinical risk, and legal confusion can be more expensive to recover from.
You can keep using telehealth — just do it smart: verify, read, ask, and save records. Regulators and industry are taking steps, but your best protection is informed action.
References & selected reading (inline, not clustered)
-
CMS — No Surprises: Understand Your Rights Against Surprise Medical Bills. Useful for billing protections and how to contest surprise charges. CMS
-
HHS Telehealth — Prescribing controlled substances via telehealth: official policy about when tele-prescribing is allowed. telehealth.hhs.gov
-
NCBI/PMC — Privacy and Security Risk Factors Related to Telehealth: systematic review of privacy/security risks. PMC
-
CMS White Paper — Exploring Fraud, Waste and Abuse within Telehealth: technical report on schemes and detection. CMS
-
Reuters reporting — telehealth & GLP-1 privacy challenges (industry/regulatory overview). Reuters
-
FTC/Consumer resources — consumer alerts and top scams (reporting guidance). Consumer Advice
FAQ
Q — Can I sue a telehealth app for privacy violations?
Potentially — depending on jurisdiction and whether the app is a HIPAA-covered entity or violated consumer protection laws. Many cases involve the FTC or state attorneys general; private lawsuits are also possible. For actionable steps, speak to a consumer attorney and document the incident.
Q — Do these risks apply to my doctor’s telehealth portal?
Less likely. Health systems typically are HIPAA-covered and use BAAs with vendors. Risks remain if third-party consumer apps are involved or if your clinician uses consumer-grade platforms without proper agreements.
Q — Will new laws force apps to stop using ad trackers?
Possible. The FTC and state privacy laws are raising the bar. Expect increased limits or requirements for consumer health data in the coming years.
Share this with someone who uses telehealth often — this loophole is small but real.